Background
The use of androgenic steroids once the domain of elite athletes and competitive body-builders, is now popular in the general population, especially among young men attending gyms.
These performance and image enhancing drugs are taken to increase muscle bulk and strength, and for faster recovery. For many men their use is associated with body dissatisfaction disorders including muscle dysmorphia, and eating disorders.
Negative body image is a primary driver for androgen use among young men.
Since men who use androgens tend not to engage with primary healthcare professionals and there is limited research in the area, the long-term side effects aren’t fully clear.
However, androgen use has been linked to serious conditions including cardiovascular disease, liver and brain damage, rhabdomyolysis and embolism. Other undesirable side effects include infertility, gynecomastia, acne and an increased risk of contracting infectious disease.
Given that the prevalence of androgen use is estimated to be 6%, this practice represents a major public health concern.
A study by Danish researchers performed a large-scale retrospective control-case study to investigate mortality and morbidity among androgen users.
Aim
To investigate long-term survival and the prevalence of co-morbidities among androgen users compared to age and gender matched controls.
Methods
Under the Danish anti-doping programme, collaborating gyms (capturing 80% of gym users in Denmark) undergo annual inspections and testing of gyms users suspected of using androgenic steroids.
Between January 2006 and March 2018, 545 men who were laboratory-confirmed androgen users were included in the study. A second validation cohort included 644 men who were strongly suspected of using androgens but refused testing.
Both cohorts were compared to age and gender matched control cohorts (n=5450 and n=6440, respectively).
Retrospective health outcomes were derived using national personal identification numbers linked to the healthcare system, and these outcomes were captured until May 2018.
The primary endpoint recorded was all-cause mortality; secondary endpoints included the incidence and prevalence of somatic co-morbidities related to androgen use.
Results
In the androgen use confirmed cohort (n=545), the average age in which men were tested positive was 26.2 years (standard deviation [SD] 6.3). The average length of follow-up was 7.4 years (SD 2.9), which was similar to the control group (7.3 years; SD 3.0).
At the end of the follow-up period, the all-cause mortality rate (primary endpoint) was seven cases (1.3%) in androgen users, compared to 23 cases (0.4%) in controls (hazard ratio [HR] 3.0; 95% CI 1.3-7.0).
Hospitalisations were higher among androgen users compared to control groups (1.26 versus 0.68 hospital contacts per person/year).
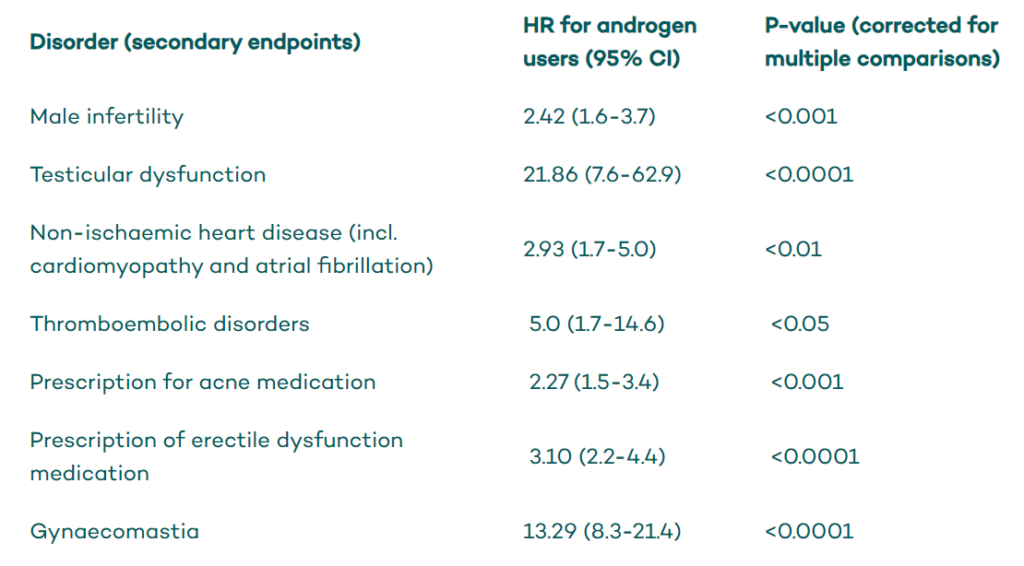
The hazard ratios (HR) for specific co-morbidities in androgen users are summarised in the following Table.
Findings related to primary and secondary endpoints were replicated in the cohort of presumed androgen users.
Conclusion
Men who use androgens have a significantly higher risk of mortality, more hospital presentations and an increased risk of multiple co-morbidities, compared to men of the same age, from the general population.














