Background
Transgender refers to someone whose gender identity does not align with their sex assigned at birth [1]. Some transgender individuals choose to undergo social or medical transition to more closely align their physical appearance with their gender identity.
Hormones may be used to suppress endogenous sex hormone secretion and to maintain sex hormone levels within the normal range for the person’s affirmed gender [2].
For trans men (referred to in the journal article as transmasculine participants) this may involve injectable or transdermal testosterone therapy, aiming for testosterone levels in the normal male range.
Trans women (referred to in the journal article as transfeminine participants) may use oestrogen alone or in combination with an antiandrogen to obtain oestradiol and testosterone levels in the normal female range [2].
Although sex at birth is an independent predictor of cardiovascular outcomes, the role played by sex hormones remains uncertain, and this uncertainty is even greater in those receiving cross sex hormone therapy [3].
Evidence for adverse effects relating to hormone therapy comes largely from studies of hypogonadal men or postmenopausal women on hormone replacement therapy. There is conflicting evidence regarding cardiovascular risk with testosterone therapy in hypogonadal men [4].
The Women’s Health Initiative trials indicated an increased risk of thrombosis and stroke in women taking oestrogen alone or with a progestogen (equine oestrogen and medroxyprogesterone acetate in this case).
An increased risk of myocardial ischaemia was also seen in women who commenced oestrogen with progesterone more than 10 years post menopause [5]. There are concerns about increased risk of thrombotic events, particularly relating to long term oestrogen therapy in trans women [2].
Aim
To compare acute cardiovascular event (ACVE) rates in a cohort of transgender persons receiving care via the Kaiser Permanente healthcare and insurance network in Georgia, and northern and southern California, USA with rates observed in age, ethnicity, site and membership matched reference men and women.
Methods
This cohort study examined the rate of ACVEs (venous thromboembolism (VTE), ischaemic stroke and myocardial infarction) in adult patients enrolled with Kaiser Permanente between 2006 and 2014.
Each transgender patient was matched to 10 reference women and 10 reference men by year of birth, ethnicity, study site and date of first episode of care. Electronic medical records were reviewed for diagnostic codes for VTE, ischaemic stroke and myocardial infarction.
History of prior ACVE, smoking status, body mass index (BMI), blood pressure and total blood cholesterol was recorded for each participant at baseline. These variables were controlled for in the analysis.
2842 trans women and 2118 trans men were identified for the study. They were matched to 48,686 reference men and 48,775 reference women. A subgroup of patients who commenced oestrogen treatment after the index date (853 of the 2842 trans women) were analysed separately as the “oestrogen initiation cohort”. Mean follow up was between 3–4 years.
Trans men undergoing treatment were younger than trans women (68% were between 18–35 years compared to 44%). There were fewer smokers in the group of reference women than the other cohorts (8.4% compared to 14–18%).
Blood pressure was elevated (>140/90mmHg) in 16% of the trans women compared to 9.3% of the trans men. Data on BMI and cholesterol was incomplete in up to 15% of participants.
Results
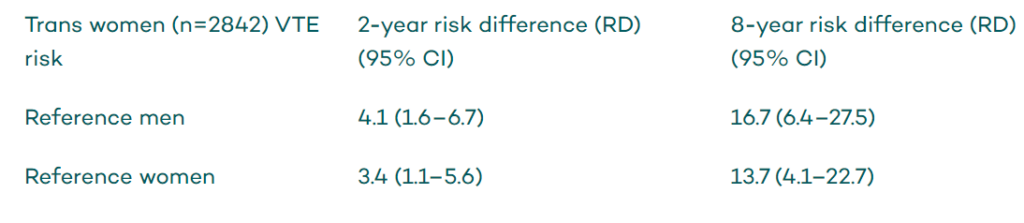
Trans women had a higher incidence of venous thromboembolism (VTE) compared reference groups:
The incidence of myocardial infarction was greater amongst trans women compared to reference women (RD 1.8; 95% CI, 1.1–2.9) but not reference men (RD 0.9; 95% CI, 0.6–1.5).
Trans women who initiated oestrogen after the index date (n=853) had a higher incidence of VTE and ischaemic stroke compared to both reference men and reference women (no difference was observed in the incidence of myocardial infarction).
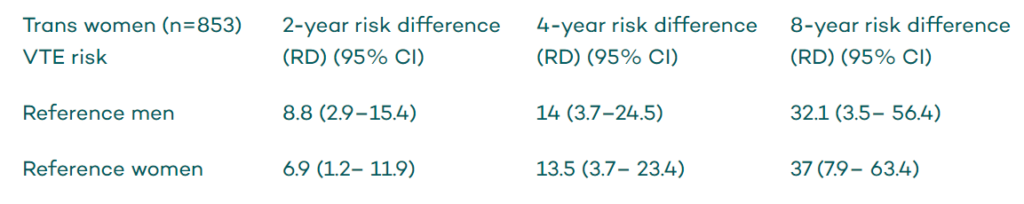
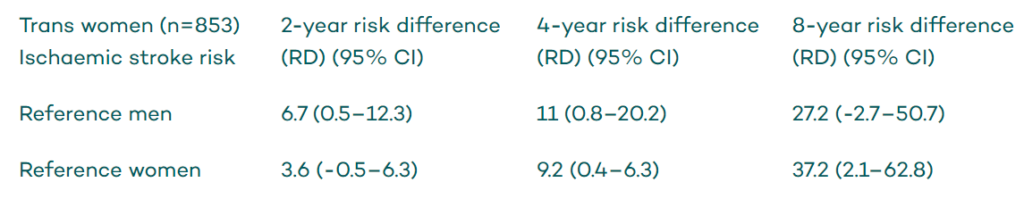
Contrary to outcomes from hormone replacement therapy in postmenopausal women, the risk difference of VTE and ischaemic stroke continued to increase with time for trans women. However, this may be a reflection of the small number of trans women with long term follow up in this cohort.
The hormone dose was only reported for the most common preparation used – oral oestradiol. The maximum average oestradiol dose was 4.1mg (range 1–10mg) in those with VTE or ischaemic stroke (n=11), a similar dose given to trans women with neither event (n=391; 4.2mg; range 0.3-10mg).
However, in those with VTE or ischaemic stroke the average dose used in the first two years of follow up was lower (3.6mg; range: 1–7mg) compared to after 2 years of follow up (5.6mg; range 2–10mg). In those with no ACVE there was no difference in mean dose before and after 2 years of follow up (4.1 vs 4.4mg).
There was no evidence for increased ACVE risk in trans men, however the number of ACVEs was low, possibly reflecting the younger age of this group.
Conclusion
This electronic medical record based cohort study of transgender persons indicates that trans women had higher rates of VTE and ischaemic stroke compared to reference men and women.
This study provides insufficient evidence to draw conclusions about increased risk for any ACVE among trans men, receiving testosterone therapy.
Reviewed by Dr Anna Watts MBBS BMedSci MPH FRACP; Dr Sonali Shah MBBS (Hons) FRACP
Health Professional Education
North Western Melbourne Primary Health Network (NWMPHN) have recently released a new Trans GP Module for GPs, nurses and medical students.














