Australia’s response to the COVID-19 pandemic undoubtedly saved hundreds, if not thousands, of lives. It showed that the coordinated efforts of government, industry, the public service, education providers and health services can respond rapidly and effectively to public health needs.
COVID-19 is a reminder that different interventions are required by different groups in our society to achieve the best health outcomes for everyone.
COVID-19 also reminds us of the health disparities between Australian men and women. In Australia and around the world, COVID-19 disproportionately affects the elderly, people with chronic disease, and men.
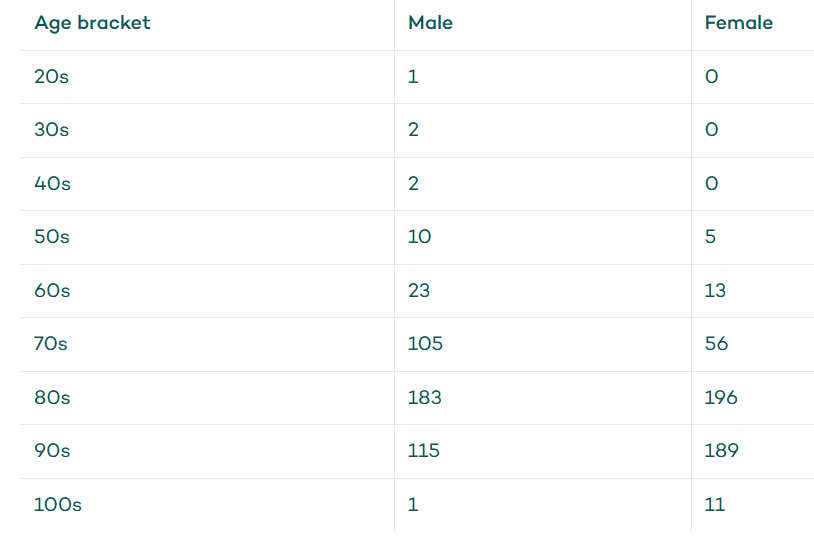
As of 28 October 20201, five Australians under 50 years of age have died of COVID-19 — all of them were male. Ten men and five women in their 50s, 23 men and 13 women in their 60s, and 105 men and 55 women in their 70s have died from the infection.
For every age group, the mortality rate is higher for men than women.
Male vs female COVID-19 mortality rate
What’s to blame?
Male susceptibility to COVID-19 is unlikely to be due to things as simple as the genetic or hormonal differences between men and women. Men’s general state of health, arising from their behaviour, might be the cause.
Men are more likely than women to have poor diets, to drink too much alcohol and smoke, to delay seeking help for health problems, and to behave in ways that puts their health at risk2.
This all adds up to a situation where Australian men have four-and-a-half fewer years of healthy life than women3.
The poor health of men doesn’t just account for their risk of dying from COVID-19. Men’s health and wellbeing is closely associated with sexual function4 and fertility5.
The physical factor
Your physical health can play a major role in having a healthy sex life and starting a family.
While the connections between our body’s various organs and systems are not always as straightforward or direct as ‘the foot bone’s connected to the leg bone’, the effects of one system on another can be strong.
In some cases, problems with sexual function can be due to the consequences of chronic disease — glucose in the urine of men with diabetes can encourage bacterial growth, leading to foreskin infections and phimosis, for example.
In other cases, the underlying problem responsible for health problems may affect the reproductive system as well as other parts of the body — for example, the nerve damage that causes multiple sclerosis can affect the nerves to the penis and cause erectile dysfunction.
The relationship between obesity and fertility in men further demonstrates the complexity of connections that can link different diseases and health conditions6.
In recent decades, as obesity rates have increased worldwide7, sperm counts have fallen8. While this might just be coincidence, there’s good reason to suspect that this global phenomenon is a consequence of men’s biology.
An analysis of data from other studies of individual men shows that, indeed, as body fat rises, fertility falls9.
Fat cells (called adipocytes) convert testosterone to estradiol (a kind of estrogen hormone), lowering the levels of the hormone that is needed for male sexual function.
Fat cells also produce a hormone called leptin, which can reduce testosterone production and sperm development. One of the effects of inflammation associated with obesity is damage to sperm, which might also account for the low sperm counts in obese men.
Mental health matters
This interplay of diseases is not just about physical ailments — it’s our mental health too.
Take erectile dysfunction, for example. Getting and maintaining an erection is complicated. It requires arousal from the brain, stimulation of nerves supplying blood vessels, and proper function of these blood vessels, to change blood flow in the penis.
If you’re depressed or anxious, getting aroused can be a challenge.
If your nerves or blood vessels are affected by diabetes, or your blood vessels’ ability to dilate is damaged, the mind might be willing but the body not able.
Regardless of the cause of your erectile dysfunction, it has considerable effects on your quality of life and can lead to depression. Depression might lead to poor diet, lack of exercise, obesity and diabetes.
Managing your health holistically
Although you might go to a specialist to help manage a specific health condition — a urologist for erectile dysfunction, an endocrinologist for diabetes, a cardiologist for heart disease, a psychologist for depression, a physiotherapist for sore joints or muscles — having a general practitioner who knows you well, who can help integrate all the information about your health and wellbeing, is really important.
Managing your health is easier when there’s cooperation and coordination between everyone who cares for you, but there needs to be someone in charge. That someone should be you.
And your team shouldn’t just be your general practitioner and other medical specialists. It should be everyone who cares for you — your physio, acupuncturist, personal trainer, the people who prepare your food, friends and family.
Think of looking after yourself as requiring the same sort of cooperation needed between all the different parts of society required to deal successfully with COVID-19. If we have a clear goal and the help we need, we can do great things.











