The GP’s role
-
Klinefelter syndrome should be considered by GPs in male patients presenting with any relevant symptoms or signs
-
Most diagnoses of Klinefelter syndrome occur either prenatally, around the expected time of puberty or in association with infertility
-
Accurate measurement of testicular volume (using an orchidometer; Image 1) during routine physical examination would likely improve detection of Klinefelter syndrome, thereby facilitating simple, effective treatment with life-long benefit
-
GPs are ideally placed to perform clinical assessments, order laboratory investigations, refer for specialist assessment and initiation of testosterone replacement therapy, and coordinate ongoing management of Klinefelter syndrome
Clinical notes
Some features of Klinefelter syndrome are related to the syndrome (e.g. behavioural and cognitive) and some features relate to androgen deficiency (e.g. osteoporosis).
Condition overview
-
Klinefelter syndrome is the most common cause of androgen deficiency in men
-
Klinefelter syndrome refers to a collection of characteristics in males caused by the presence of two or more X chromosomes
-
The most common (80-90%) karyotype of males with Klinefelter syndrome is 47,XXY. Some males with Klinefelter syndrome have more than two X chromosomes, or chromosomal mosaicism
-
Klinefelter syndrome prevalence is estimated to be 1 in 500 males, with only around half of those affected ever diagnosed
-
Klinefelter syndrome is characterised by impaired testosterone production and spermatogenesis
-
Classical features of Klinefelter syndrome (Image 2) are present to differing degrees in individuals
-
The only consistent feature of Klinefelter syndrome is small testes volume (< 4 mL)
-
The subtle effects of Klinefelter syndrome in many men account for low rates of diagnosis and illustrates the importance of genital examination as part of routine clinical exams
-
Men with Klinefelter syndrome benefit from testosterone replacement therapy
-
Infertility is common in men with Klinefelter syndrome, due to oligi- or azoospermia, but paternity may be possible with assisted reproductive technologies using sperm collected by microdissection testicular sperm extraction (microTESE)


Image 1 – 30mL (normal)(left)/4mL (Klinefelter syndrome)(right)
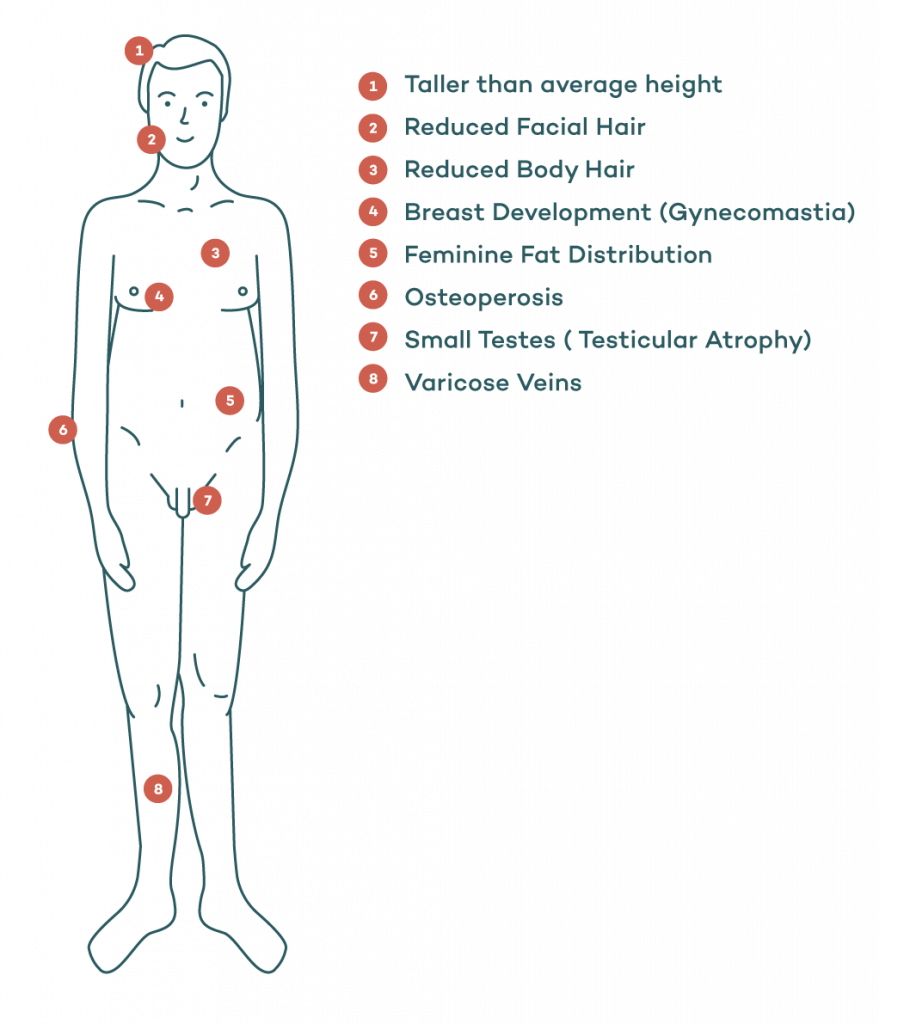
Image 2 – Clinical features of Klinefelter syndrome. Features present may be few, some or all.
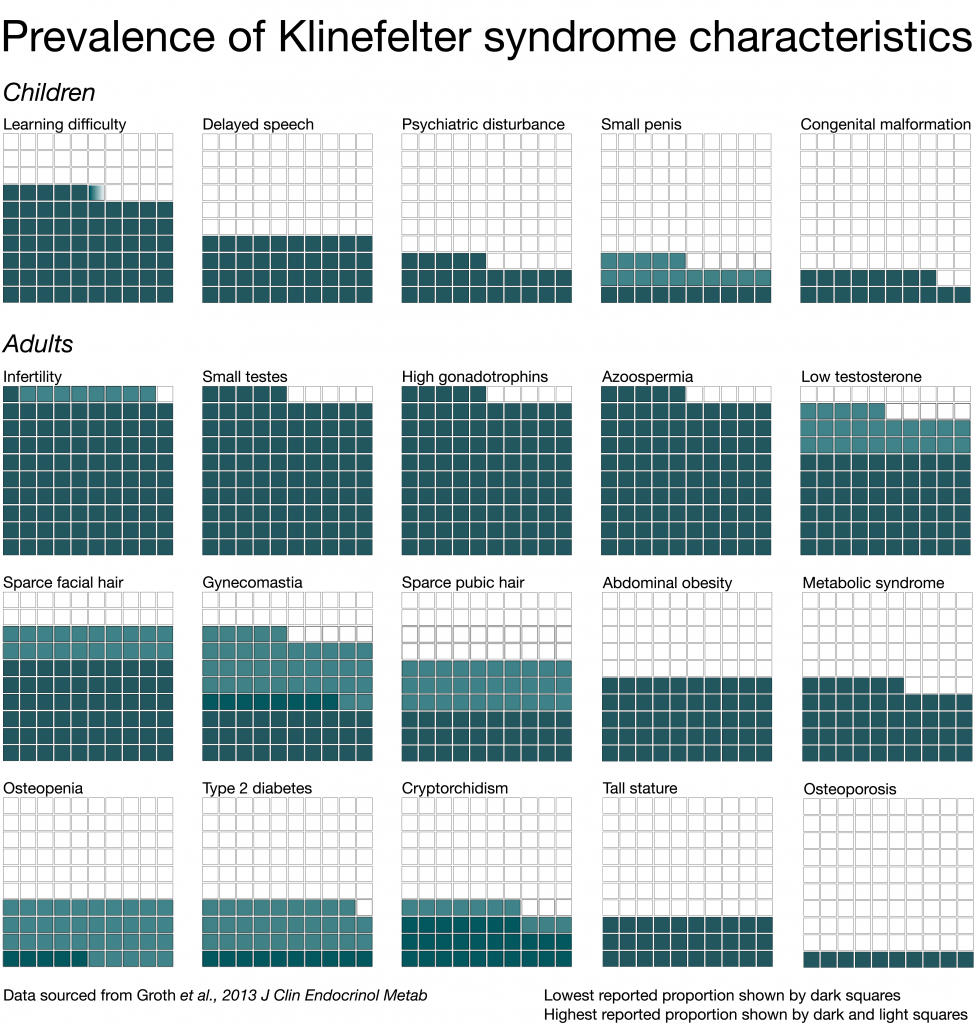
Image 3 – Prevalence of Klinefelter syndrome characteristics
Diagnosis
-
Medical history
1. Pubertal development (poor progression)
2. Sexual function (low libido)
3. Degree of virilisation
4. Psychosocial (learning, schooling and behaviour)
5. Infertility
-
Examination
-
Infancy
1. No hormonal features prior to puberty
2. Undescended testes
3. Rarely, ambiguous genitalia
-
Adolescence
1. Small testes (< 4 mL) are a characteristic feature from mid puberty
2. Poor pubertal progression and facial, body and pubic hair relative to age
3. Gynaecomastia
4. Feminine fat distribution
5. Taller than average height
6. Poor muscle development
-
Adult
1. Small testes (typically < 4 mL)
2. Reduced facial, body and pubic hair
3. Gynecomastia
4. Feminine fat distribution and weight gain
5. Taller than average height
6. Poor muscle development
Testicular volume
-
Assessment of testicular volume is essential
Testicular volume is assessed using an orchidometer
Normal testicular volume range:
– Childhood 3 mL or smaller
– Puberty 4–14 mL
– Adulthood 15–35 mLSmall testes:
– 4 mL is the only consistent feature of Klinefelter syndrome (Image 2)The testes may start to develop in early puberty, but soon regress to 4 mL by mid puberty
-
Investigations
Two fasting, morning samples of serum total testosterone, taken on different days
Total serum testosterone, low or low normal from mid puberty (normal range typically 8–27 nmol/L)
Serum LH, elevated from mid puberty (normal range 1-8 IU/L)
Serum FSH, elevated from mid puberty (normal range 1-8 IU/L)
Karyotype (47,XXY)
– 10% mosaic 46,XY/47,XXY -
Other investigations (reason/risk)
Bone densitometry, DEXA (osteoporosis)
Semen analysis if fertility is an issue (usually azoospermic)
Thyroid function tests (hypothyroidism)
Fasting blood glucose (diabetes)
| T formulation | Usual (starting) dosage | Dosage range | Comment |
|---|---|---|---|
| Injections (IM) | |||
| Testosterone undecanoate | 1000mg every 12 weeks following loading dose at 6 weeks (i.e., 0, 6, 18, 30 weeks) | Longer term: typically 500-100mg at 8 to 16-week intervals | |
| Combined testosterone propionate Testosterone phenylpropionate Testosterone isocaproate Testosterone decanoate* Testosterone enantate* | 250mg every 2 weeks | 10- to 21-day intervals | These preparations are not typically prescribed in adult men |
| Transdermal gel | |||
| Testosterone (1% as 50 mg in 5 g sachet OR 12.5 mg/ actuation pump pack dispenser; applied daily) | 50mg daily | 25-100mg daily | |
| Testosterone (2% as pump dispenser; applied daily) | 50mg daily | 25-100mg daily | |
| Transdermal cream | |||
| Testosterone 5% cream | 25mg (0.5mL) daily applied to scrotum | Up to 50mg (1mL) daily (to scrotum) | PBS listing now requires scrotal application |
| Transdermal patch | |||
| Testosterone* | 5mg applied nightly | 2.5 to 5mg daily | |
| Oral undecanoate | |||
| Testosterone undecanoate* | 40mg capsule 160-240mg in 2 to 3 doses daily | 80 to 240mg daily |
Management
Testosterone replacement therapy (TRT)
-
TRT is lifelong and may be started from mid puberty, although many boys initially virilise normally
-
Gynecomastia is an indication to start TRT (see below)
-
Teenage boys usually start on a low dose and build to full adult dose as puberty progresses
-
Even if measured testosterone concentrations are normal, there is evidence that bone density is reduced in the presence of chronically raised LH levels, suggesting that TRT is indicated
-
In adults, consult with a fertility specialist (if appropriate) to develop a plan for fertility preservation prior to TRT, as TRT will suppress spermatogenesis
Gynaecomastia
-
Gynaecomastia may be transient, lasting one to three years
-
Adequate testosterone replacement often results in complete resolution over 12 months
-
Surgical removal, mastectomy (do not refer for early surgery as it may resolve naturally or following TRT)
Follow-up
Monitoring TRT is essential.
-
Prostate
Men with Klinefelter syndrome are less likely to die from prostate cancer, and restoring testosterone levels to the normal range is likely only to return their risks to those of their eugonadal peers
Subject to the same advice about testing for prostate cancer as their peers (PSA)
Exclusion of significant prostate pathology is essential for those aged >40 years at the commencement of therapy
-
Raising clinical awareness
Aside from cognitive and behavioural features, it is important to note that despite the following recognised disease associations with Klinefelter syndrome, the absolute risk is low
Tumours: leukaemia, mediastinal germ cell tumours, lymphoma, teratoma and breast cancer
Endocrine: hypothyroidism and diabetes mellitus
(Type 1 is rare and Type 2 is often affected by obesity)Cardiovascular: venous ulcers and venous thromboembolic disease
Auto-immune: systemic lupus erythematosis (SLE) and coeliac disease
Referral
Children and adolescents
-
Refer to a paediatric endocrinologist
-
Refer for educational and allied health assistance if needed
Adults
-
Develop a plan in consultation with an endocrinologist for assessment and management of:
– Hormone deficiency
– Infertility
– Osteoporosis
– Cardiovascular risk -
Refer to a fertility specialist +/- urologist, as appropriate, for sperm recovery from testis or donor sperm
Fertility
Infertility is a major implication of Klinefelter syndrome.
-
Most men are azoospermic
-
Sperm are rarely found in the ejaculate but in 30-50% of cases sperm can be found with microdissection testicular sperm extraction. Access to surgical expertise and high costs can make this prohibitive for many affected men. Where sperm is found, Intracytoplasmic Sperm Injection (ICSI) fertility treatment would be required
-
Treatment options:
ICSI — the risk of 47,XXY offspring is low
Donor insemination
-
Counselling may be necessary
Learning and behaviour difficulties
The general intellectual ability of boys with Klinefelter syndrome is within the normal range. However, boys with Klinefelter syndrome may have:
-
Difficulties with speech and reading
-
Delayed motor development
-
Reduced attention span
-
Behavioural problems (particularly in adolescence)
-
Requirement for educational and allied health assistance
Clinical review
Dr Rita Upreti, Endocrinologist, Monash Health and Hudson Institute of Medical Research










